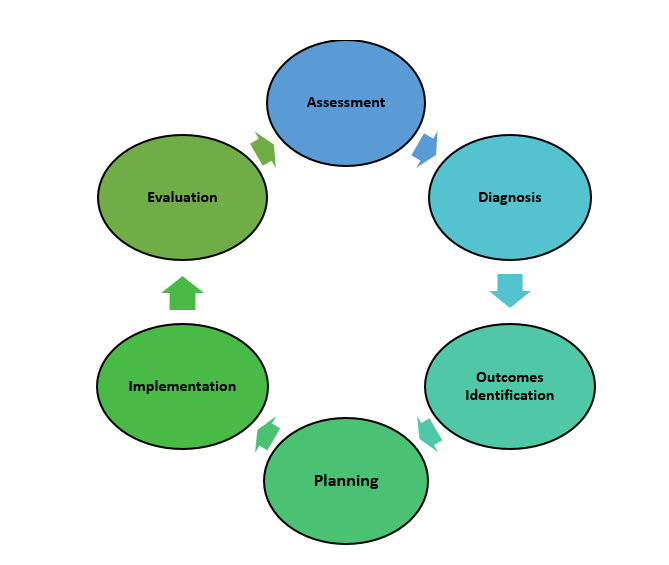
The is a critical thinking model based on a systematic approach to patient-centered care that nurses use to perform clinical reasoning and make clinical judgments when providing patient care. The nursing process is based on the Standards of Professional Nursing Practice established by the American Nurses Association (ANA). These standards are authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently.[1] The mnemonic ADOPIE is an easy way to remember the ANA Standards and the nursing process, with each letter referring to the six components of the nursing process: Assessment, Diagnosis, Outcomes Identification, Planning, Implementation, and Evaluation. See an illustration of the cyclical nursing process in Figure 2.3.[2]
The Assessment component of the nursing process is defined as, “The registered nurse collects pertinent data and information relative to the health care consumer’s health or the situation.”[3] A nursing assessment includes physiological data, as well as psychological, sociocultural, spiritual, economic, and lifestyle data. Nursing assistants should observe and report things to the nurse that they notice when providing care, such as reddened or open skin, confusion, increased swelling, or reports of pain.[4]
The Diagnosis phase of the nursing process is defined as, “The registered nurse analyzes the assessment data to determine actual or potential diagnoses, problems, and issues.”[5] A nursing diagnosis is the nurse’s clinical judgment about the client’s response to actual or potential health conditions or needs. Nursing diagnoses are the basis for the nursing care plans and are different than medical diagnoses.[6]
The Outcomes Identification phase of the nursing process is defined as, “The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation.”[7] The nurse sets measurable and achievable short- and long-term goals and specific outcomes in collaboration with the patient based on their assessment data and nursing diagnoses.[8] Nurses may communicate expected outcomes to nursing assistants, such as, “The client will walk at least 100 feet today.”
The Planning phase of the nursing process is defined as, “The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes.” Assessment data, nursing diagnoses, and goals are used to select evidence-based nursing interventions customized to each patient’s needs and concerns. Goals and nursing interventions are documented in the patient’s nursing care plan so that nurses, as well as other health professionals, have access to it for continuity of care.[9]
Nursing care plans are part of the Planning step of the nursing process. A nursing care plan is a type of documentation created by registered nurses (RNs) that describes the individualized planning and delivery of nursing care for each specific patient using the nursing process. guide the care provided to each patient across shifts so care is consistent among health care personnel. Some nursing interventions can be assigned or delegated to licensed practical nurses (LPNs) or nursing assistants with the RN’s supervision.[10] Although nursing assistants do not create or edit care plans, they review this document to know what care should be provided to each client within their scope of practice.
The Implementation phase of the nursing process is defined as, “The nurse implements the identified plan.”[11] Nursing interventions are implemented or delegated with supervision according to the care plan to assure continuity of care across multiple nurses and health professionals caring for the patient. Interventions are also documented in the patient’s medical record as they are completed.[12] The nursing assistant’s largest responsibility during the nursing process is safely implementing their delegated interventions in the nursing care plan.
The Evaluation phase of the nursing process is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.”[13] During evaluation, nurses assess the patient and compare the findings against the initial assessment to determine the effectiveness of the interventions and overall nursing care plan. Both the patient’s status and the effectiveness of the nursing care must be continuously evaluated and modified as needed. To assist the nurse in evaluation, nursing assistants must report any changes in patient condition or new observations related to new interventions. Because nursing assistants spend the most time with the residents, it is important to communicate with the nurse if asked to implement an intervention that is known to be ineffective with a resident so a different, more effective alternative can be identified.
Using the nursing process has many benefits for all members of the health care team. The benefits of using the nursing process include the following[14]: